Heart failure is a serious medical condition that occurs when the heart is unable to pump blood efficiently to meet the body’s needs. This can lead to a variety of symptoms and complications if left untreated. Understanding the signs, when to seek medical advice, and the treatment options available can empower individuals to manage their heart health more effectively.
Table of Contents
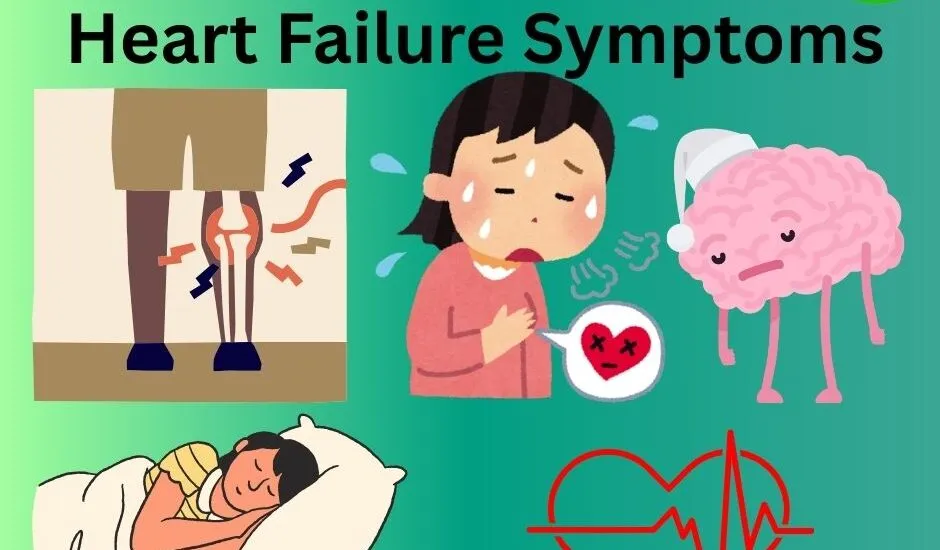
Symptoms of Heart Failure
The symptoms of heart failure can vary widely among individuals, and they may develop gradually or appear suddenly. Recognizing these signs is crucial for early intervention and effective management. Below are expanded descriptions of the common symptoms:
1. Shortness of Breath: This symptom may manifest during physical activity, such as climbing stairs or walking, but it can also occur at rest. Individuals may notice increased difficulty breathing when lying flat, known as orthopnea, or experience paroxysmal nocturnal dyspnea, where they wake up suddenly feeling breathless in the middle of the night.
2. Fatigue: Heart failure often leads to decreased blood flow to the muscles and organs, resulting in a general feeling of tiredness. People may find themselves needing to rest frequently, feeling drained after minimal exertion, or experiencing a lack of energy to engage in activities they previously enjoyed.
3. Swelling (Edema): Fluid retention can occur in various parts of the body. Swelling in the legs, ankles, and feet is common as gravity causes fluid to pool when standing or sitting. Abdominal swelling due to fluid buildup can lead to discomfort, bloating, and changes in appetite.
4. Rapid or Irregular Heartbeat: Also known as palpitations, this symptom may feel like the heart is racing, pounding, or fluttering. These changes in heart rhythm can be unsettling and may be accompanied by feelings of anxiety or unease, reflecting the heart’s attempt to compensate for its decreased pumping efficiency.
5. Persistent Cough or Wheezing: A chronic cough, often accompanied by sputum that may be white or pink-tinged, can be a sign of fluid accumulation in the lungs. Wheezing may also occur, indicating restricted airflow, and can cause discomfort, especially during physical activities.
6. Increased Need to Urinate: Many individuals with heart failure experience nocturia, which is the increased need to urinate during the night. This symptom is often due to the body redistributing fluids when lying down, leading to increased urine production.
7. Lack of Appetite: People with heart failure may experience gastrointestinal symptoms, including a diminished appetite or feelings of fullness after eating only a small amount. This can be related to fluid retention in the abdomen and reduced blood flow to the digestive system.
8. Confusion or Impaired Thinking: Reduced blood flow to the brain can lead to cognitive issues. Individuals may experience confusion, memory problems, or difficulty concentrating, making it essential for caregivers and loved ones to be aware of these changes.
9. Sleep Disturbances: Besides shortness of breath, individuals may experience increased anxiety at bedtime or find it hard to maintain a restful sleep. This can lead to a cycle of fatigue and further exacerbate other symptoms.
10. Chest Discomfort: Some people may experience discomfort or a feeling of pressure in the chest, which can be concerning and may resemble symptoms associated with heart attacks. It’s important to note that any new or severe chest discomfort should be evaluated immediately.
11. Cold Extremities: In some cases, reduced circulation can cause the hands and feet to feel unusually cold or clammy. This can occur along with other symptoms, such as pallor or changes in skin color.
When to See a Doctor
If you experience any of these symptoms, especially if they are new or worsening, it’s essential to consult a healthcare professional. Early detection is crucial for effective treatment and management. Seek immediate medical attention if you experience:
– Sudden or severe shortness of breath
– Chest pain
– Fainting or severe dizziness
– Rapid or irregular heartbeat
Testing and Diagnosis
To diagnose heart failure, healthcare providers may perform several tests, which may include:
1. Physical Examination: The doctor will check for signs of heart failure, such as swelling, elevated jugular vein pressure, or abnormal heart sounds.
2. Blood Tests: These can help determine heart function and identify any underlying issues.
3. Electrocardiogram (ECG or EKG): This test measures the electrical activity of the heart to detect abnormalities.
4. Echocardiogram: A key diagnostic tool, this ultrasound test provides images of the heart’s structure and function.
5. Chest X-ray: This can reveal if there is fluid buildup in the lungs or enlargement of the heart.
6. Stress Test: This assesses how the heart functions during physical exertion.
7. Cardiac MRI or CT Scan: These imaging tests can provide detailed information about the heart’s structure and function.
Treatment Options
While heart failure is a chronic condition, it can be managed effectively with a combination of lifestyle changes, medications, and sometimes surgical interventions. Treatment plans are tailored to individual needs and may include:
1. Medications: Common medications for heart failure include:
– Diuretics (to reduce fluid buildup)
– ACE inhibitors or ARBs (to lower blood pressure and improve heart function)
– Beta-blockers (to slow the heart rate and lower blood pressure)
– Aldosterone antagonists (to help prevent fluid retention)
2. Lifestyle Modifications:
– Diet: Adopting a heart-healthy diet low in salt, saturated fats, and sugars.
– Exercise: Engaging in regular, gentle exercise as recommended by a healthcare provider.
– Weight Management: Maintaining a healthy weight can lessen the burden on the heart.
– Quitting Smoking and Limiting Alcohol: These measures can significantly improve heart health.
3. Device Therapy: In some cases, devices like implantable cardioverter-defibrillators (ICDs) or cardiac resynchronization therapy (CRT) may be recommended.
4. Surgical Interventions: Depending on the cause of heart failure, surgery may be necessary to repair damaged heart valves or to bypass blocked arteries.
Conclusion
Heart failure is a complex condition that requires ongoing management. By being aware of the symptoms, knowing when to seek help, and understanding the diagnostic and treatment options available, individuals can take proactive steps toward improving their heart health. If you or someone you know is experiencing symptoms of heart failure, don’t hesitate to reach out to a healthcare professional for guidance and support.
Contact us at 406-272-2376orschedule online.